Asthma in Pregnancy
)
I well remember a maternal death from asthma in Dublin during a Caesarean section. The anaesthetists were devastated.
What may have caused that was the use of ergometrine after the baby was delivered. This is a risk factor for bronchoconstriction especially when general anaesthesia is combined. In my experience that fact is not well appreciated by clinicians.
In Australia 12.7% of pregnant women suffer asthma.
One in 9 Australians suffer from asthma: a chronic inflammatory disorder of the airways. Atopy, the genetic predisposition for the development of an immunoglobulin E (IgE)-mediated response to common aeroallergens, is the strongest identifiable predisposing factor for developing asthma. Viral respiratory infections are one of the most important causes of asthma exacerbation and may also contribute to the development of asthma. Airway inflammation contributes to airway hyperresponsiveness, airflow limitation, respiratory symptoms, and disease chronicity. In some patients, persistent changes in airway structure occur, including sub-basement fibrosis, mucus hypersecretion, injury to epithelial cells, smooth muscle hypertrophy, and angiogenesis.
Acute symptoms of asthma usually arise from bronchospasm and require and respond to bronchodilator therapy. Acute and chronic inflammation can affect not only the airway calibre and airflow but also underlying bronchial hyperresponsiveness, which enhances susceptibility to bronchospasm.
The four pathophysiological processes in asthma include: a) broncho-constriction; b) oedema of airways c) airway hyper-responsiveness and d) airway remodelling. It is this last process which has become better appreciated: permanent structural changes can occur in the airway these are associated with a progressive loss of lung function that is not prevented by or fully reversed by current therapy.
Drugs in pregnancy which can precipitate asthma include ergometrine, NSAID’s, asprin ,ACE inhibitors (although these should be ceased in any pregnancy because of an increased risk of fetal renal impairment and fetal death) carbetocin, prostaglandin F2 alpha (but not Cervidil ™or Prostin E2™).
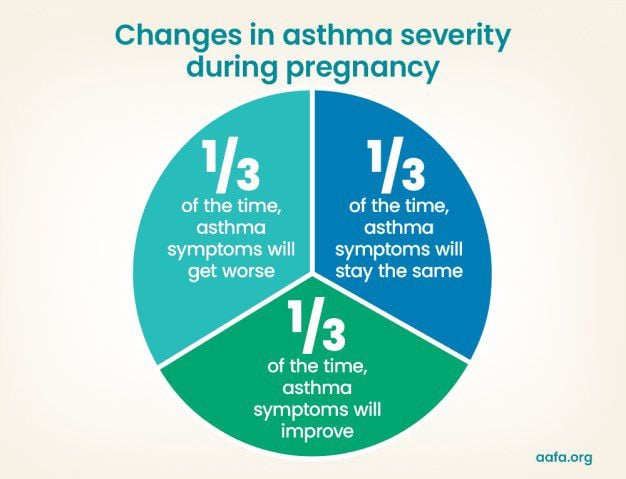
The majority of women with asthma have normal pregnancies and the risk of complications is small in those with well-controlled asthma . According to Schatz et al.. , approximately 1/3 of asthmatic pregnant women experience an improvement of asthma during pregnancy, 1/3 remain stable and 1/3 of women experience a deterioration of asthma.
During pregnancy the cornerstone of asthma treatment is the use of relievers (short-acting beta agonists such as Ventolin™) and preventers especially inhaled corticosteroids such as budesonide (Pulmicort™) or Sym-bicort ™ which contains budesonide and formoterol- a long acting beta agonist.
Effects of Asthma in Pregnancy
Asthma is associated with increased risks of peri-natal mortality (OR 1.24), preterm birth (OR 1.18, low birth weight(OR:1.29), fetal growth restriction (SGA) (OR: 1.26) , and asphyxia (OR 1.37) . Asthma treatment reduces the risk of preterm delivery, but it does not seem to reduce other complications such as perinatal mortality
The odds risk of preterm delivery for untreated mothers is 1.31 :this is reduced to an odds ratio for 1 medication of 1,19 and for 2 medications the OR is 1.06.
Deaths from Asthma: New 2023 Australian data show an increase in deaths from asthma of 30% since 2022.From 2018 to 2020 there were 3 maternal deaths in Australia from preexisting respiratory disease.
Smoking in asthmatic mothers
There appears to be an increased preva-lence of smoking in Australian females with asthma even during pregnancy as evidenced by a retrospective study con-ducted in 2009 ( Clifton VL et al,2009)in which 1944 pregnant women with asthma and 13,977 pregnant women without asthma were included. Exacer-bations were more frequent in current smokers (52%) and ex-smokers (48%) compared with never smokers (35%), . Risk factors for exacerbations during pregnancy include smoking, obesity and respiratory virus infection. Clearly smoking is a preventable factor.
Inhaled corticosteroids remain the on-ly treatment that clearly reduces acute asthma exacerbations and asthma mor-tality for people in all asthma age groups six years and older and should be used in the majority of people with asthma.
Further Reading:
- National Asthma Education and Prevention Program, Third Expert Panel on the Diagnosis and Management of Asthma. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Bethesda (MD): National Heart, Lung, and Blood Institute (US); 2007 Aug. Section 2, Definition, Pathophysiology and Pathogenesis of Asthma, and Natural History of Asthma. Available from: https://www.ncbi.nlm.nih.gov/books/NBK7223/
- Cohn L, Elias JA, Chupp GL. Asthma: mechanisms of disease persistence and progression. Annu Rev Immu-nol. 2004;22:789-815. Review
- National Heart, Lung, and Blood Institute, National Asthma Education and Prevention Program Asthma and Pregnancy Working Group. Managing asthma during pregnancy: recommendations for pharmacologic treatment-2004 update. J Allergy Clin Immunol 2005; 115: 34-46.
- Schatz M, Harden K, Forsythe A, et al. The course of asthma during pregnancy, post partum, and with successive preg-nancies: A prospective analysis. J Allergy Clin Immunol. 1988;3:495-504
) Author:Dr Mike O'Connor
Author:Dr Mike O'Connor







