NIPT screening & Nuchal Translucency - Complimentary rather than alternatives
The advent of the Non Invasive Prenatal Test has been a major advance for the detection of Trisomy 21 (Down s.), Trisomy 18 (Edwards s.) & Trisomy 13 (Patau s.) and reduces the need for invasive tests which have up to a 3% risk of miscarriage.
There has been a subsequent tendency to abandon the previous nuchal translucency ultrasound and biochemical test because of the increased accuracy of detection of the trisomies with the NIPT test which can detect 99% of Down syndrome fetuses c.f. a 90% detection rate with NT Plus.
What seems to be less well appreciated is that the NIPT does not provide a full karyotype as it relies on frag-ments of fetal DNA within maternal blood .These are then used to detect T211,T18 or T13 using specific probes. More recently a further probe is availa-ble to detect 22 q deletions as found in DiGeorge syndrome: a complex syndrome involving cardiac ,facial, skeletal and neurological abnormalities which has an incidence of 1/1000.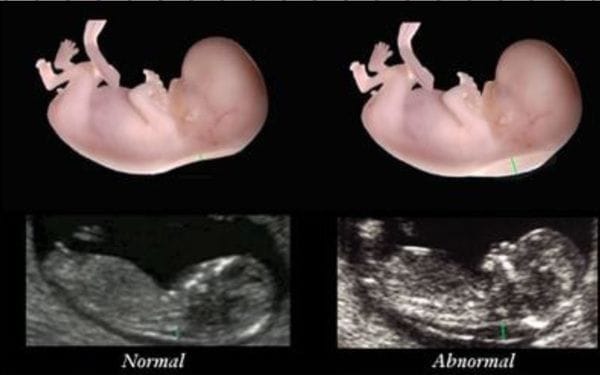
Reliance on an NIPT to exclude a fetal aneuploidy is unsound and a positive NIPT will still require confirmation using genetic amniocentesis or CVS. The value of a nuchal translucency test between 11-13 weeks is that it will give additional information not available with an NIPT test.
For example, the nuchal translucency is not just increased (>3 mm) in fetal aneuploidies such as Down syndrome and Turner's syndrome (45 XO) but is also increased in fetal cardiac malformations: more than 55% of all major congenital heart defects in one series (Hyett et al 1999) had an NT > 95 per-centile (NR 1.8-2.35 mm) and the negative predictive value of a normal NT was 99.9%.
Furthermore a careful ultrasound scan at 11-13 weeks can give additional information such as cervical length ( values <3 cm can predict cer-vical incompetence) as well as basic information such as cranial anatomy (eg excluding anencephaly), spine, stomach, kidneys, bladder & presence of all 4 limbs. These non-cardiac features can be reasonably assessed in between 75-98% of cases between 11-14 weeks. Other important ultrasound findings at 11-13 weeks include detection of uterine fibroids and ovarian tumours which may cause complications such as red degeneration and torsion respectively later in pregnancy.
Fetal morphology scans: diagnostic value and limitations especially fetal heart anomalies
The fetal morphology scan is normally performed between 18-20 weeks gestation. If performed by skilled ultrasonologists it will detect a significant number of serious fetal anomalies. It is important to remember that only about one third of structural abnormalities are associated with an abnormal karyotype. The basic information available includes:
- An assessment of gestational age (+/- 7-10 days error)
- An assessment of fetal morphology
- An assessment of placental localization (bearing in mind that the vast majority of 'low lying' placentae will not remain so by term)
Approximately 1% of liveborn fetuses have congenital heart disease (CHD). What is concerning is the failure to diagnose a large number of these fetuses with (CHD) at that gestational age. A little later at 22 weeks there is a better yield of diagnoses of CHD.
The 1993 RADIUS study surveyed 92 obstetric practices and 17 family practices in 6 US States and identified 15,530 low risk pregnant women who were scanned between 15-22 weeks and 31-35 weeks by 28 ultrasound referral laboratories staffed by 91 qualified sonologists. Of those women (whose fetal anomaly rate was 2.3%) only one third had one (or more) major fetal anomalies detected by 24 weeks. It demonstrated that few of the CHD's were detected .No improvement in overall perinatal outcome could be demonstrated.
More recently one US study (Pinto et al, 2011) over a 10 year period found that only only 39% of 1474 cases of significant CHD were detected, with no improvement in detection rate over the 10year period. Detailed fetal echocardiography can improve the detection rate but this is impractical for large populations. The 4 chamber cardiac scan is the basic standard and this will miss defects such as transposition of the great arteries (TGA), tetralogy of Fallot (TOF), double-outlet right ventricle (DORV) and truncus arteriosus. The 4 chamber view cardiac view is likely to identify complete atrioventricular septal defect (AVSD), congenitally corrected transposition of the great arteries (CCTGA), tricuspid valve disease (including Ebstein's anomaly) and all single ventricle defects including hypoplastic left heart syndrome (HLHS). A circumspect approach is therefore required when receiving a normal fetal morphology scan result.
Further reading:
- Alldred SK et al. First trimester ultrasound tests alone or in combination with first trimester serum tests for Down's syndrome screening.Cochrane Database Syst Rev. 2017 Mar 15;3:CD012600. doi: 10.1002/14651858.CD012600.
- Sharifzadeh M et al. Normal reference range of fetal nuchal translucency thickness in pregnant women in the first trimester, one center study J Res Med Sci. 2015 Oct; 20(10): 969973.
- Hyett J,Perdu M,Sharland G, Snijders R,Nicolaides K. Using fetal nuchal translucency to screen for major congenital cardiac defects at 10-14 weeks of gestation: population based cohort study BMJ. 1999 Jan 9; 318(7176): 8185.
- Pinto NM et al. Barriers to prenatal detection of congenital heart disease: a populationbased study Ultrasound Obstet Gynecol. 2012 Oct;40(4):418-25. doi: 10.1002/uog.10116. Epub 2012 Sep 17.
- Ewigman BG et al. Effect of prenatal ultrasound screening on perinatal outcome. RADIUS Study Group.N Engl J Med. 1993 Sep 16;329(12):821-7.
| Tags:UltrasoundMiscarriageObstetrcis |








