NIPT testing has significant diagnostic limitations
The advent of NIPT testing in 2011 in Hong Kong was a breakthrough after many years of fruitless research which focussed on examining complete fetal cells in the maternal blood. Only one fetal cell is usually present per 1 ml of maternal blood. By contrast there are approximately 4.5 x 106 maternal red cells per ml of maternal blood. So it was like looking for a needle in a haystack!
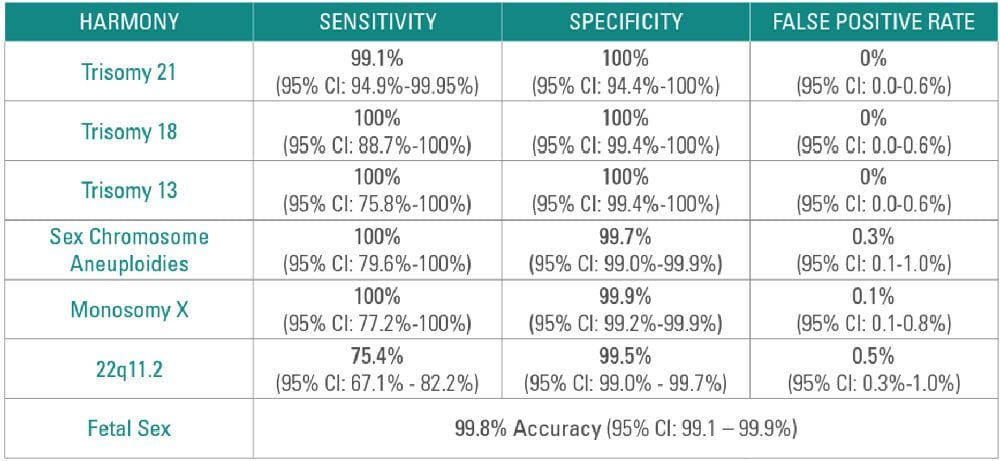
Non-invasive prenatal testing (NIPT) has revolutionized the prenatal screening landscape with its high accuracy and low false positive rate for detecting Trisomy 21, 18 and 13.
The new technology uses the detection of fragments of fetal DNA in the maternal circulation which are amplified using PCR techniques.
The key fetal aneuploidies which can be diagnosed are Down syndrome/ Trisomy 21 (99% detected) Edwards syndrome/ Trisomy 18 ( 93% detected) and Patau syndrome /Trisomy 13 (92% detected) as well as abnormal numbers of X or Y chromosomes (sex chromosome aneuploidy) such as Turner syndrome (X0) and Kleinfelter’s syndrome (XXY).
There is also the potential to diagnose 22q deletions such as a majority of DiGeorge syndrome( which includes congenital heart defects, unusual facies and cleft palate, loss of vision and hearing & developmental delays).
The problem arises when NIPT test is portrayed as a more comprehensive test than it really is. Ultrasonic fetal morphology examinations at 18-20 weeks should be seen as essential and complementary.
The aneuploidy risks of advanced maternal age include Trisomy 21 (Down) Trisomy 18 (Edwards) and Trisomy 13 (Pateau) + Trisomies 15, 22 and 14 and XXX (associated with cognitive disorders and hypotonia) and XXY ( Kleinfelter’ syndromes-associated with feminisation of males who are infertile).
CCell-free DNA (cfDNA) are small fragments which usually contain 150-180 DNA building blocks (base pairs) and arise when cells die off and get broken down and their contents including DNA, are released into the bloodstream. Analysing cfDNA from the placenta provides an opportunity for early detection of certain genetic abnormalities without harming the fetus.
NIPT for fetal aneuploidy employs high throughput sequencing methods (“next generation sequencing") to count the proportional representation of each chromosome in the plasma cfDNA. In a euploid pregnant woman, a deviation from the expected chromosome profile in plasma cfDNA due to excess or deficient cfDNA fragments from a particular chromosome suggests the presence of fetal trisomy or monosomy, respectively.
NIPT can be performed in twin pregnancies. Although this is associated with a higher test failure rate, studies suggest that NIPT’s sensitivity for T21 is similar for twin and singleton pregnancies.
NIPT may include screening for additional chromosomal disorders s that are caused by missing (deleted) or copied (duplicated) sections of a chromosome.
There must be enough fetal cfDNA in the mother’s bloodstream to be able to identify fetal chromosome abnormalities. The proportion of cfDNA in maternal blood that comes from the placenta is known as the fetal fraction. Generally, the fetal fraction must be above 4 percent, which typically occurs around the tenth week of pregnancy. Low fetal fractions can lead to an inability to perform the test or a false negative result. Reasons for low fetal fractions include testing too early in the pregnancy; sampling errors; maternal obesity & fetal abnormality.
NIPT for other monogenetic syndromes
NIPT can be used to test for genetic disorders that are caused by changes (variants) in single genes. Inherited monogenic diseases such as DiGeorge syndrome (22q); haemophilia, sickle cell anaemia; achondroplasia and thanatophoric dwarfism have all been detected using Next Generation Sequencing involving targeted locus amplification with microarray technology .Fragile X detection is not possible as the 1000 base pair repeats are not found in cfDNA.
Test manufacturers offer other options such as tests for rarer trisomies, copy number variants, and microdeletions, including 15q deletion (Prader–Willi and Angelman syndromes), 4p deletion (Wolf– Hirschhorn syndrome), 15p deletion (cri-du-chat syndrome), and 11q deletion ( Jacobsen syndrome), but the sensitivity and positive predictive value for these conditions are significantly lower and there is a risk of increasing the overall false-positive rate when screening for more conditions.
The most recent prenatal screening guidelines from the American College of Obstetricians and Gynecologists do not recommend using NIPT for these rarer conditions due to a lack of evidence regarding validity.